This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
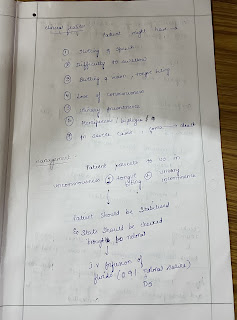
55 year old female came with chief complaints of
• Fever since 4 days
• SOB since 4 days
HOPI: The patient was apparently asymptomatic 4 days back , then developed she had a H/o RTA ( Fracture of left lowerlimb) S/p wound debridement with external fixator under spinal anaesthesia)
H/o pus discharge from external fixator site.
Grade 4 SOB progressive in nature ( At rest) a/w lower back ache and generalised body pains.
, progressive in nature
, high grade , relieved on medication.
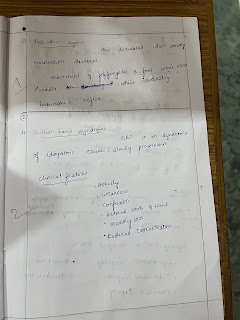
PAST HISTORY: k/c/o Diabetes mellitus 2
Not a K/c/o HTN, TB,CVA ,CAD ,Epilepsy ,Asthma
PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
B&B: Regular
Addictions: No addictions.
O/E
General examination
Temp: 98.9 F
PR: 100 bpm
BP: 130/90 mm hg
RR: 22 cpm
SpO2: 98% @ RA
GRBS: 387 mg / dl
Systemic examination
CVS: S1S2 + , No murmurs
RS: BAE + , NVBS
P/A: Soft , NT
CNS: No FND
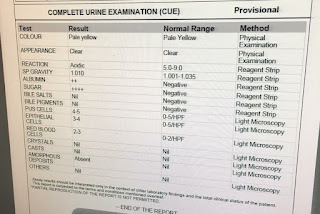
INVESTIGATIONS
TREATMENT:
IVF NS & RL continuous infusion @ 180 ml/hr
Inj. HAI 8 units/IV/STAT
Inj. HAI 10 ml in 39 ml NS IV @ 6ml/hr
Inj. MEROPENEM 1gm IV/BD
Inj. VANCOMYCIN 1 gm in 100 ml NS IV/BD
Inj. PAN 40mg IV/OD
GRBS Monitoring hourly
IVF 25% Dextrose if GRBS is more than 150 mg/dl.